Tips to Improve Immunity
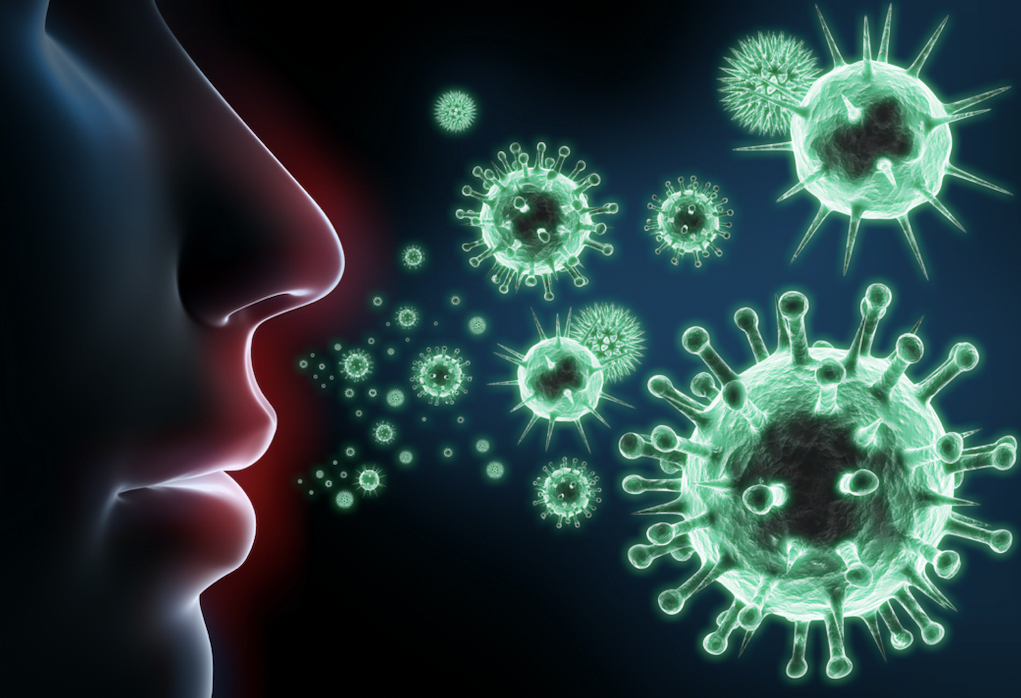
Our amazing immune system has evolved over millions of years to protect the body from the daily attacks from bacteria, viruses, fungi and parasites. A healthy immune system also detects and kills the estimated 3000 mutated cells which make it past the DNA repair mechanisms each day – meaning it also protects us from cancer. In this post we will discuss in detail on lifestyle tips to improve immunity.
Problems with the immune system can stem from the system itself being deficient, in which case there is an increased risk of infection and cancer, or due to the system being overactive, whereby an exaggerated immune response results in an over-reaction to innocuous allergens such as dust, pollen or some foods, leading to asthma, eczema or food allergies. An overactive immune system, in the long-term, can lead to a state of chronic inflammation which leads to an increased risk of oxidative stress and chronic degenerative disorders such as dementia, high BP, Dupuytren’s and arthritis.
|
Factors which can damage the immune system
|
Factors which can enhance the immune system
|

Smoking and pro-inflammatory chemicals: As well as promoting chronic inflammation, toxins in smoke and food can also damage innate protective mechanisms such as the cilia hairs within the lining of the airways responsible for moving mucous (containing viruses) out of the body. Smoking also causes irritation and thinning of the tissues lining the nose and throat, making it easier for viruses to penetrate the cells (tips to quit smoking).
Obesity: Being significantly overweight inevitably leads to a state of chronic inflammation. Obesity leads to trauma to cells(which are more fragile), suboptimal gut health, an increased risk of urinary tract infections, fungus growth within the skin folds, and an even greater risk of psychological disturbances, all of which can affect inflammatory regulation (tips to lose weight effectively).
Micronutrient imbalances: Poor dietary choices can contribute to imbalances in essential minerals and vitamins. Deficiencies or excesses in essential micronutrients can cause sub-acute illness which reduce the immune system’s functioning and lead to high levels of inflammation. Try to diversify your diet with foods rich in minerals and vitamins or even consider micro-nutrient testing.


Lifestyle Tips to Improve Immunity
Gut health, food intolerances and the microbiome: There is a critical and complex relationship between our immune system and the trillions of microbes in the body. The biodiversity of gut and skin bacteria deteriorates with age, obesity, poor diet, sedentary behaviour, food intolerances and low intake of polyphenols. This leads to a decrease in the protective healthy bacteria within the skin, nose, mouth, mucous membranes and gut. Low levels of good bacteria increase the risk of infection but also allow proliferation of bad pro-inflammatory bacteria which damage the linings of our body – thinning the skin and mucous membranes and increasing permeability (leaky gut syndrome), enabling infections to enter the bloodstream quicker. This leaky gut syndrome also increases the influx of toxins into the blood, which in turn cause direct damage to tissues such as joints, muscles, the heart and the brain (read the benefits of probiotic bacteria).
Processed sugar: Some dietitians and health professional mistakenly believe that processed sugar and other high-glycaemic-index (GI) foods, such as refined carbohydrates, only cause inflammation by contributing to weight gain. In reality, sugar feeds unhealthy gut bacteria, leading to poor gut health and local then systemic inflammation. A wealth of robust scientific data explains the multiple mechanisms by which sugar damages our bodies (tips to reduce sugar intake).
Psychological stress: Chronic stress produces a hormone called cortisol that is released by the adrenal glands. Stress initially reduces immunity and inflammation but, in the long-run, chronically high cortisol disrupt blood sugar balance, often leading to high insulin levels, obesity and sometimes diabetes, all of which increase the wrong type of inflammatory markers (tips to improve psychological wellbeing).
Exercise and immunity: Regular and sensible exercise increases levels of catecholamines which stimulate the recruitment of immune cells (white blood cells) and natural killer (NK) cells into the peripheral blood and tissues. This is particularly important for obese individuals and the elderly, whose immune function becomes less efficient with age (read more about the benefits of exercise).
Polyunsaturated fatty acids (PUFA): These are a good source of slow-release energy, have important roles in many essential biochemical pathways and are required to build cell walls. Both omega 3 and 6, found in fish, healthy nuts and vegetable oils, help regulate inflammatory processes and responses by producing anti-inflammatory fats. They are an essential component for an appropriate immune cascade (read about healthy and unhealthy fats).


Appendix: Background – Our immune system in a nutshell
The immune system is split into an early (acute) system which forms a barrier to try and stop an infection growing or spreading, and an acquired targeted system which kills infections and stores information which enables a quick response next time the body is exposed to the same bugs.
 The acute (innate) immune system
The acute (innate) immune system
Your body’s first line of defence is the barrier of the skin and mucous membranes lining the mouth, lungs, gut and vagina, all of which prevent bugs from entering the body. It includes chemical substances like gastric acid, surface enzymes and mucus which stop bacteria from entering the body, while movements created by hair-like structures in the bronchi also stop germs from settling. The innate system also recruits trillions of friendly bacteria present on our skin and gut to actively fight off nasty pathogens and take up space which harmful organisms would otherwise occupy. These friendly bacteria also have a significant role in alerting the immune system when the body is under attack.
The second component of the innate system is the acute inflammation response, initiated by cells such as mast cells – the whistle-blowers of the acute immunity system – in response to injury, invading pathogens, or the recognition of cells that are perceived to be hostile. These cells release inflammatory signalling chemicals (cytokines) such as histamines, serotonin and prostaglandins which are responsible for the local signs and symptoms of inflammation we are all familiar with. It is not quite clear why these chemicals make us feel so unwell, but one theory is that it discourages people from moving about, preventing mixing with others and potentially spreading the germs.
The innate response promotes infiltration of white cells and natural killer (NK) cells into the affected area of the body. These identify cells that are, either infected, have become cancerous or are perceived as foreign, and then produce local toxins which kill them. At the same time, they release further chemical signals (cytokines) into the bloodstream, triggering the next phase of the immune system’s attack – the processes of acquired immunity.
The acquired (adaptive) immunity system
Unlike the innate immune system, the adaptive immune system is very efficient at killing specific bugs, foreign particles or pathogens. It does this in two phases; first, molecules called antibody responses (produced via white cells known as B-cells) travel through the bloodstream and bind to the proteins on the surface of the pathogen, otherwise known as antigens. This binding then triggers cell-mediated immunity, which involves activation of the immune system’s lethal army of phagocytes and killer T-lymphocytes. After bugs or foreign cells have been killed, the template for these antigens are stored in memory cells which means that next time the bugs attack, instead of taking 5-7 days, the body is able to launch a specific, targetted attack in hours. This “immunity” can also be acquired by an artificial vaccination such as the flu jab.




 The acute (innate) immune system
The acute (innate) immune system