The risks of excess sugar explained By Professor Robert Thomas
.
There remains considerable confusion in the media and debate among health professionals regarding the link between high processed sugar intake and an elevated risk of cancer. The misunderstanding arises mainly because many critics of the association fail to emphasise that it’s not sugar itself which is harmful, but rather the habit of eating or drinking processed sugar and refined carbohydrates. Normal levels of sugar in our bloodstream do not cause or promote cancer. In fact, sugar helps feed every cell in the body, together with other energy sources such as fatty acids and ketones. Sugar is so important to the function of the brain and other organs that the body has several back up strategies to keep blood sugar levels normal.

Types and sources of common sugars and carbohydrates
Carbohydrates, or saccharides to use their scientific name, are molecules consisting of rings of carbon, hydrogen and hydrogen atoms. They are important sources of energy for the body and are divided into four main chemical groups.
Monosaccharides: Glucose, fructose, galactose and xylose. The latter two are rarely found naturally on their own. Small amounts of free natural glucose can be found in figs, sweet corn, grapes, mango and bananas. Fructose is more commonly found in fruit such as apples, fig, grapes, pears, honey and some root vegetables. The majority of glucose and fructose we eat is added by the manufacturer.
Disaccharides: Sucrose (a fusion of glucose and fructose) is table sugar and is the usual sugar added to sweets, candies, sugary drinks, toffees, pastries, cakes, doughnuts and processed foods. Sucrose is harvested from sugar cane or sugar beet. Lactose (glucose and galactose) is the sugar found in milk. People with lactose intolerance lack the enzyme which breaks down the bond between glucose and galactose to enable its absorption. Maltose (glucose and glucose), found in malted drinks and beer, can be found naturally in cereals.
Oligosaccharides: These are intermediate chain carbohydrates found in artichoke, burdock, chicory, leeks, asparagus and onions. They are commonly used as food additives as they give food and drinks a smooth, more substantial texture. The most commonly used oligosaccharide additives include maltodextrins, inulin and oligofructose. They are sometimes referred to as soluble fibres or prebiotics because they are not easily broken down in the small bowel and 90% pass to the large bowel, providing energy for the commensal bacteria. As a consequence, in their natural forms, they are generally regarded as beneficial as they enhance a healthy gut flora.
Polysaccharides: These include starch, amylose, cellulose and pectins. Starch is the most common carbohydrate in the human diet and is found in many staple foods. The major sources of starch are cereals (rice, wheat, maize, oats, millet, barley) and any foods made from them such as bread, pasta, chips, cakes and noodles. They are also found in root vegetables such as potatoes, carrots, cassava, swede, sweet potato, yams and legumes. These complex polysaccharide-containing foods, in their natural form, tend to contain other nutrients such as fibre, proteins, vitamins and minerals which are not only healthy for the body but also moderate the transit of food through the gut, slowing the stomach emptying time and delaying the breakdown and absorption of glucose. Unfortunately, processing these foods often removes many of these healthy elements and increases their breakdown and absorption times, thus increasing their GI.
Fructose versus glucose: A common misconception is that fructose has less of a negative impact on the body than glucose. This confusion probably arises because fructose is the most common sugar in fruit, which have numerous other nutritional benefits. The other complication is that fructose, unlike glucose, is less likely to trigger an insulin increase as insulin is not required for its metabolism. Unfortunately, excess fructose intake is just as harmful as glucose. In one laboratory experiment, rhesus monkeys fed a human-like, high fructose diet developed diabetes within 3 months [Bremer]. In humans, 4 weeks of a diet high in processed fructose led to an increase in signs of insulin resistance [Silbernagel], while several other studies have linked a high fructose diet (>50g/day) with hypertension, obesity, metabolic syndrome [Johnson, Livesey], raised uric acid and type 2 diabetes [Johnson].

- Dried fruit: The process of drying and processing the fruit removes water and damages some of the nutrients, but more importantly, significantly concentrates the fructose content. Some manufacturers also add more sugar and sulphites for taste and preservation. The table below highlights the 5-6 fold increase in sugar because of this process (e.g. fresh figs – 7%, dried figs – 55%). On the positive side, despite this high sugar content, they still have fibre, polyphenols and pulp, so their GI is still lower than an equivalent processed food with similar levels of sugar.
- Fruit juices: Many of the fruit juices on the market aren’t even “real” fruit juices. They consist of water, mixed with concentrate and extra sugar. Even 100% real fruit juice still has a high concentration of fructose because so many more fruits are used. A 300ml orange juice containing 4-5 oranges can quite easily have the same sugar content as a fizzy cola drink. There is also little chewing resistance to slow down consumption, making it very easy to consume a large amount of sugar in a short period of time. This lack of pulp significantly speeds up gastric emptying and GI. There is certainly some truth in the commonly used Californian expression “Eat your fruit – Juice your vegetables”
- Smoothies: Those which involve the whole fruit being put into the blender are better as they maintain the pulp and fibre. They still have a high fructose content, especially if sugary fruits such as grapes, pears, apples and mangos are used. To overcome this, smoothie aficionados often add fruits which are less sweet such as avocado, vegetables such as kale, and spices such as ginger, all of which lower the sugar content and enhance the polyphenol content.
Other factors which lower GI
As well as the type of carbohydrate, the timing and total content of the entire meal influences GI. Wholemeal bread has a slower absorption, as well as more vitamins and fibre than typical thin white, while wholemeal or fava bean enriched pasta, as well as al dente pasta, have a slower GI than overcooked white pasta [Tunco]. Processed sugars on an empty stomach, such as first thing in the morning, are particularly harmful as they are absorbed rapidly. Conversely, a small sweet dish after a healthy meal will have less of an impact as the stomach has plenty of other food to slow the gut down.
 Phytochemicals reduce the impact of sugar
Phytochemicals reduce the impact of sugar
It has long been known that a higher intake of polyphenol-rich foods is linked to a lower risk of type two diabetes T2D [Bi, Xiao], primarily because they are capable of lowering blood sugar levels. The underlying mechanisms of how they achieve this include inhibition of α-amylase and α-glucosidase, inhibition of glucose absorption in the intestine by sodium-dependent glucose transporter 1, stimulation of insulin secretion and reduction hepatic glucose output.
.
Cancer promoting mechanisms of sugar
High GI foods or meals with a high GL increase the cancer risk either directly, by influencing chemicals which promote cancer development and growth, or indirectly, by contributing to the development of diseases which then influence on cancer.
Direct mechanisms
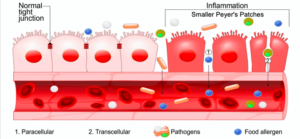
Inflammation: Several laboratory studies have shown that high GI foods promote cancer growth directly. One study involved mice with implanted breast cancer being fed sucrose with their usual meal at comparable levels to a Western diet. The western diet led to increased tumour growth and metastasis to the lung and liver when compared with mice fed a non-sugar starch diet [Yang 2015]. This effect was ascribed to increased expression of inflammatory markers, including 12-lipoxygenase (12-LOX) and its arachidonate metabolites [Yang 2015].
Insulin-like growth factor (IGF): High sugar and insulin levels lead to direct overproduction of IGF, a hormone which activates several signalling pathways, leading to the inhibition of apoptosis, the promotion of cell growth and angiogenesis [Yu, Frierer]. Higher levels of IGF-1 in humans are associated with a greater cancer risk [Ryan, Ma]. Two large international studies involving people with treated bowel cancer both reported those who eat higher GL diets had higher average IGF levels and an increased relapse rate after primary surgery and chemotherapy [Palmqvist, Meyerhardt].
Genetic damage: Studies have found that high sugar levels can result in the formation of oxidative metabolites which increase intracellular free radicals [Bucala]. Laboratory experiments involving flies deficient in Vitamin B6 (more susceptible to genetic damage) reported that feeding them with pure sugar led to significantly higher direct DNA damage and chromosome instability [Marzio].
Indirect mechanisms
Epidemiological studies have independently linked high GI foods with a significant risk of obesity, diabetes, dental caries and depression, which, in turn, contribute to the risk of subsequent cancer and poorer outcomes after cancer treatments.
Obesity: Sugary drinks pack on the pounds because this high energy source is less satiating (signalling to the body to stop eating when you have had enough calories), resulting in higher consumption. Sugary drinks or meals also trigger a damaging yo-yo effect on blood glucose and insulin levels. The body responds to an initial sugar rush by rapidly increasing insulin levels, metabolising excess sugar into energy storage such as glycogen in the liver. As sugar has only been around in the human diet for the last 150 years, our body thinks that this level of sugar hitting the bloodstream must be associated with a very large meal, so it produces excess insulin which then causes sugar levels to drop and stimulates hunger and fatigue. The natural reaction to this is to reach for another high calorific snack or drink, which provides instant relief but starts the process all over again. Obesity, especially in postmenopausal women, increases levels of oestrogen, insulin-like Growth factor (IGF) and other hormones such as leptin, all of which have been shown in laboratory experiments to increase proliferation and spread of cancer cells. Fortunately, in terms of weight control, it’s never too late to cut out sugar. A meta-analysis of 68 studies showed that individuals who embarked on diet plans which replaced sugar for more slow-release energy sources experienced a significant decrease in body weight. Losing weight, fasting and exercise are associated with a lowering of IGF levels, oestrogen and a decreased breast cancer risk.
Diabetes and glucose intolerance: Independent from the risk from obesity, high sugar intake directly increases the risk of diabetes by overloading the insulin pathways. Individuals with T2D have higher serum insulin levels (hyperinsulinemia) due to the pancreas producing excessive amounts in order to overcome cellular insulin resistance. High serum insulin levels are considered to be a major risk factor for cancer development, largely because of insulin receptor stimulation on cancer cells. In addition, hyperglycemia-related oxidative stress and low-grade chronic inflammation, both of which are associated with diabetes, promote malignant transformation. It is not a surprise, therefore, that a study involving 872,706 Australians found a significant link between T2D and fatal cancer. The American Diabetes Association and the American Cancer Society have issued a consensus report stating that 2TD leads to a two-fold higher risk for cancers of the liver, pancreas, and endometrium, and a 1.5-fold increased risk for cancers of the colon and rectum, breast, bladder and leukaemia.
Depression: An analysis of data from participants within the Whitehall Cohort reported that those with a high consumption of sugary drinks, sweetened desserts, chocolates, processed meat and fried foods had a 58% increased risk of depression. That said, it’s hard to establish whether depression is the cause or effect of high sugar consumption, with low mood arguably encouraging people to consume sugary foods as part of a quick-fix aimed at feeling better. Depression is also linked to increased risk of serious cancers. One study, which followed men with prostate cancer from California, identified that men with an associated depressive illness were more likely to die specifically of prostate cancer than those with normal mental health.
Insomnia: Sleep slows the cell cycle which helps DNA repair, reboots energy stores and clears out toxins which have built up over the day. Chronically poor sleep adversely effects gut health, impairs immune function, interferes with melatonin release and hence interferes with a normal circadian rhythm (read more). A correlation between processes sugar and poor sleep patterns was identified in number of studies including one involving 100 students using food frequency and sleep quality questionnaires in the weeks leading up to their exams [Alahmary]
Cholesterol: A USA study analysed the dietary habits of a cohort of 6,110 Americans. It found that those who ate more than 10% of their daily calories as sugar had significantly higher LDL and lower HDL (good) cholesterol. As well as elevating the risk of cardiovascular disease, this lipid pattern is known to be an increased risk factor for prostate and breast cancer independent of other lifestyle habits.
Dental caries: Sugar consumption is a major cause of tooth decay, especially boiled sweets, toffees and sugary drinks. What is less well known is that dental caries may also lead to an increased risk of bowel cancer. Two studies from Canada and the USA looked at more than 100 samples of healthy and cancerous bowel tissue between them and their findings in the journal, Genome. They both found that DNA codes from bacteria, commonly found in dental caries (Fusobacterium) was present in the bowel cancer genes but not normal genes. This suggests that the bacterial DNA travelling through the body interacts with and gets absorbed into gut cells, causing them to become cancerous. Dental caries is also a prominent source of chronic inflammation.
.
Clinical evidence of a link between processed sugar intake and cancer risk
Despite the extent of the direct and indirect mechanisms via which sugar intake can cause harm, cynics still argue that, as there is a lack of randomised controlled trials (RCT), the link cannot be substantiated in humans. Although RCTs are the “gold standard” of evidence, not all lifestyle factors can be assessed in this design. It would be near impossible to randomise two large groups of individuals to eat either a diet high in sugar or no sugar at all, in order to find out if the cancer risk is different several years later. Likewise, asking people living with cancer to be randomised to a high-sugar diet or not, to see if it affects the cure rate, is unfeasible. In both scenarios, people will simply eat what they want after the first few weeks, making any results meaningless. Despite the deficit in RCTs, there is still an enormous amount of clinical data from large, well-conducted environmental and prospective cohort studies measuring their lifestyle habits and recording disease incidence and outcomes. Strong between high sugar intake have been found with several cancers including breast, prostate, oesophagus, colon and pancreas. A good systemic review of the international evidence has been written by Epner et al. Examples of the most prominent are summarised here:
- A combined analysis of the Nurses’ Health Study (NHS) and the HPFS provided data on 100,000 participants for up to 20 years. The 1,809 people who developed colorectal cancer had a history of higher intake of processed carbohydrates and sugar compared to people without cancer. The effect of these foods was worse in men who were overweight [Michaud 2005].
- A cohort study from Iowa (USA) evaluated 35,215 women for 10 years. The 212 cases of colon cancer had a higher intake of sucrose-containing foods and beverages other than ice cream/milk products. Again, this risk was worse in those who were overweight and curiously people who were taller [Bostick].
- Further analysis of the NHS identified 180 cases of pancreatic cancer. Those, particularly women, who were overweight and sedentary with a habit of eating meals with a high GL had a 53% increased cancer risk [Michaud].
- A study from Minnesota looked at the dietary habits of 60,000 adults from Singapore for 14 years. Drinking >2 sugary drinks/week doubled the risk of any cancer and increased risk of pancreatic cancer by 87% [Mueller].
.
How to reduce sugar intake
It is particularly important to stop sugary consuming fizzy drinks, boiled and chewy sweets, and adding sugar to tea and coffee, or cereals, cakes or muffins which are high in sugar. Most sugary foods can be easily identified, as advertisers usually label them as “Luxury” or use terms such as “treat yourself”. Maybe it’s time for governments to step in with legislation and force advertisers to tell the truth. “Treating yourself to fatigue, dental caries, obesity, heart disease, diabetes and cancer”, doesn’t have quite the same ring to it. The sugar tax is a step in the right direction but the money raised should directly subsidise healthy drinks and foods.
Sometimes it’s not so obvious whether sugar has been added, especially as some of these foods may be advertised as healthy – reduced fat ready meals, salad dressings, pasta sources, yoghurt, breakfast cereals or muesli for instance. It is worth reading the label of processed foods such as “ready meals” which typically have sugar added in order to enhance the flavour. Some restaurants add sugar to their curries and stews – you can instruct the waiter to ask the chef to omit the sugar.
The cancernet.co.uk blog has a series of practical recipes which are both delicious and contain no sugar. They also emphasise phytochemical-rich foods which, as mentioned above, also reduce the GI. A number of natural nutritionists update the blog monthly with fresh ideas supported by a short video clip explaining how the dishes are made.
Diabetic treatments and cancer
Numerous epidemiologic studies and subsequent meta-analyses have repeatedly indicated that T2DM patients receiving metformin, compared to those taking other anti-diabetic medications, have a decreased risk of various types of cancers [Kasznicki, Quinn]. Most notably, in the UK, a total of 62,809 patients with diabetes were found to have a higher risk of pancreatic cancer, particularly if also obese, but a lower risk if they were taking metformin monotherapy as opposed to gliclazide or insulin[Curie, 2012]. This finding was substantiated by a pooled analysis of 108,161 patients with T2D, which reported that metformin treatment was associated with a significantly lower risk of colorectal cancer [Zhang]. Data from 3,837 patients obtained from several databases from Canada noted that a longer duration of metformin after diagnosis of prostate cancer was associated with a lower mortality rate [Margel]. In the US-based Women’s Health Initiative clinical trials which examined 68,019 postmenopausal women, those with diabetes had a lower risk of breast cancer if taking metformin [Chlebowski].
One proposed indirect mechanism for metformin’s benefit lies in the fact that it improves cellular sensitivity to insulin and hence reduces IGF in those developing insulin resistance [Yu]. Other studies have demonstrated a direct anticancer effect via inhibition of mTORC1, a protein complex which plays a pivotal role in metabolism, proliferation and antiestrogen hormone resistance in breast cancer cells. Metformin is thought to inhibit mTORC1, which plays a pivotal role in the metabolism, growth and proliferation of cancer cells [Chiang].
Conclusion
The link between sugar and cancer is becoming increasingly convincing. More research is clearly needed, but people who argue against the risks of processed sugar intake should realise that it is not possible to design RCTs for every scenario. The conclusion, based on existing evidence, is that it is extremely likely that regular high sugar intake leads to an increased risk of many diseases and, what’s more, no study to date has ever suggested sugar is healthy.
Many would also argue it should be up to the sugar industry to fund trials rather than continue to promote its use, especially as sugar is widely available, cheap and its consumption is growing rapidly. Since the 1960s, global sugar consumption has grown from 50 million tonnes to 180 million. Curbing global sugar consumption should be a major priority for governments, but as individuals, we can exert consumer power and simply avoid buying sugary foods, a move which will inevitably force the food industry to stop cramming sugar into anything they can.
Further reading and references:
Book – “How to Live”
Blog – tips to reduce sugar intake
Epner M, et al. Understanding the Link between Sugar and Cancer: A Cancers (Basel). 2022 8;14(24):6042. doi: 10.3390/cancers14246042.
Alahmary et al (2019) Relationship Between Added Sugar Intake and Sleep Quality Among University Students: Am J Lifestyle Med. 23;16(1):122-129.
Akbaraly T, Brunner E, Ferrie J et al. Dietary pattern and depressive symptoms in middle age. The British Journal of Psychiatry 2009, 195 (5) 408-413.
Basu S, Yoffe P, Hills N et al. The Relationship of Sugar to Population-Level Diabetes Prevalence: An Econometric Analysis of Repeated Cross-Sectional Data Plos 2013. DOI: 10.1371/journal.pone.0057873
Bi X, Lim J, Chritiani J et al Spices in the management of diabetes. Food Chemistry. 2017 Vol 217; pp281-293.
Bostick R, Potter J, Sellers T et al Sugar, meat, and fat intake, and non-dietary risk factors for colon cancer incidence in Iowa women Cancer Causes & Control 1994, 5 (1), pp38-52.
Bremer A, Kimber S, Graham J et al Fructose-fed rhesus monkeys: A nonhuman primate model of insulin resistance, metabolic syndrome, and type 2 diabetes. Clin Transl Sci. 2011; 4(4): 243-252.
Bucala R, Armitage P & Doll R et al. Modification of DNA by reducing sugars: a possible mechanism of nucleic acid aging, age-related dysfunction in gene expression. 1984, Proc Natl Acad Sci USA 81;105-109.
Burt BA and Pai S. Sugar consumption and caries risk: a systematic review. J Dent Educ 2001; 65: 1017-23.
Calle EE and Kaaks R. Obesity, hormones and cancer; epidemiological evidence and proposed mechanism. Nature Reviews Cancer 2004, 4, 579-591.
Chiang GG, Abraham RT.. Targeting the mTOR signaling network in cancer. Trends Mol Med 2007;13:433-42.
Chlebowski RT, McTiernan A, Wactawski-Wende J, et al. Diabetes, Metformin, and Breast Cancer in Postmenopausal Women. J Clin Oncol 2012;30:2844-52.
Currie C, Poole C and Gale E et al. The influence of glucose-lowering therapies on cancer risk in type 2 diabetesDiabetologia 2009, 52, (9) 17-66-77.
Currie CJ, Poole CD, Jenkins-Jones S et al Mortality after incident cancer in people with and without type 2 diabetes: impact of metformin on survival. Diabetes Care. 2012; 35(2):299-304.
DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 2000;24:794-800
Dembinska-Kiec A, Mykkänen O, Kiec-Wilk B et al . Antioxidant phytochemicals against type 2 diabetes. Br J Nutr. 2008;99:es109–ES117.
Evans JL, Goldfine ID, Maddux BA, Grodsky GM. Oxidative stress and stress-activated signaling pathways: a unifying hypothesis of type 2 diabetes. Endocr Rev. 2002;23:599–622
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE. Adult weight change and risk of postmenopausal breast cancer. JAMA. 2006;296(2):193–201.
Freedland SJ, Aronson WJ, Kane CJ et al Impact of obesity on biochemical control after radical prostatectomy for clinically localised prostate cancer:. JCO 2011; 22(3) 446-53
Freier S, Weiss O, Eran M, et al.; Expression of the insulin-like growth factors and their receptors in adenocarcinoma of the colon. Gut 1999; 44: 704-708.
Giovannucci E, Harlan E, Archer E et al. Diabetes and cancer: a consensus report. Diabetes Care 2010: 33(7): 1674-85.
Harding J, Shaw J, Peeters A et al Age-Specific Trends From 2000-2011 in All-Cause and Cause-Specific Mortality iin Diabetes: The Million People Study. Diabetes Care. 2016: 39(6): 1018-26.
Harvie M, Howell A. Energy restriction and the prevention of breast cancer. Proc Nutr Soc. 2012;71(2):263–75.
Harvie M, Sims A, Pegington M et al. Intermittent energy restriction induces changes in breast gene expression and systemic metabolism 2016 Breast Cancer Research 18:57
Harvie M et al. Association of gain and loss of weight before and after menopause with risk breast cancer in the Iowa women’s health study. Cancer Epidemiol Biomarkers Prev. 2005;14(3):656–61.
Huang Z, Hankinson SE, Colditz GA, Stampfer MJ, Hunter DJ, Manson JE, et al. Dual effects of weight and weight gain on breast cancer risk. JAMA. 1997;278(17):1407–11.
Johnson R, Segal MS, Sautin Y, et al. Potential role of sugar (fructose) in the epidemic of diabetes, kidney disease, and cardiovascular disease. Am J Clin Nutr. 2007;86:899-906.
Johnston K, Sharp P, Clifford M Dietary polyphenols decrease glucose uptake by human intestinal Caco-2 cells FEBS letters 2005; 576 (7), pp 1653-1657
Johnson R, Perez-Pozo SE, Sautin YY et al. Hypothesis: could excessive fructose intake and uric acid cause type 2 diabetes? Endocr Rev 2009;30:96-116.
Kasznicki J, Sliwininska A and Drzewoski J. Metformin in cancer prevention and therapy. Ann Trasl Med. 2014;2(6):57-61
Knekt P, Kumpulainen J, Jarvinen R, et al. Flavonoid intake and risk of chronic diseases. Am. J. Clin. Nutr. 2002;76:560–568
Kim Y, Keogh L, Clifton P. Polyphenols and glycemic control. Nutrients 2016 5;8(1).
Kitahara C, de González B, Jee S et al Total Cholesterol and Cancer Risk in a Large Prospective Study. 2011 J Clin Oncol 29:1592-98.
Kostic A, Ojesina A, Pedamallu C et al. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma18, 2011, doi: 10.1101/gr.126573.111
Te Morenga L, Mallard S, Jim Mann J et al Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies BMJ 2013;346:e7492
Livesey G and Taylor R. Fructose consumption and consequences for glycation, plasma triacylglycerol, and body weight: meta-analyses Am J Clin Nutr2008;88:1419-37.
Lorenzi M, Montisano DF, Toledo S et al. High glucose induces DNA damage in cultured human endothelial cells. 1986. L clin Invest 77(1) 322-25.
Margel D, Urbach DR, Lipscombe LL, et al. Metformin use and all-cause and prostate cancer-specific mortality among men with diabetes. J Clin Oncol 2013;31:3069-75.
Marinac CR, Nelson SH, Breen CI, Hartman SJ, Natarajan L, Pierce JP, Flatt SW, Sears DD, Patterson RE. Prolonged Nightly Fasting and Breast Cancer Prognosis. JAMA Oncol. 2016;2(8):1049-1055.
Marzio A, Merigliano C, Gatti M et al. Sugar and Chromosome Stability: Clastogenic Effects of Sugars in Vitamin B6-Deficient Cells PLoS Genet. 2014; 10(3): e1004199.
Meyerhardt JA, Sato K, Niedzwiecki D. Dietary glycemic load and cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Natl Cancer Inst. 2012 21;104(22):1702-11.
Michaud D, Fuchs C, Liu S et al. Sugar, and Colorectal Cancer Risk in Men and Women cancer Epidemiol Biomarkers Prev January 2005 14; 138.
Michaud D and Liu et al Dietary Sugar, Glycemic Load, and Pancreatic Cancer Risk in a Prospective Study JNCI J Natl Cancer Inst (2002) 94 (17): 1293-1300.
Mueller N, Odegaard A, Anderson K et al Soft drink and juice consumption and risk of pancreatic cancer: the Singapore Chinese Health Study. Cancer Epidemiol Biomarkers Prev. 2010; 19(2):447-55.
Ma J, Pollak M, Giovannucci E et al. Prospective study of colorectal cancer risk in men and plasma levels of Insulin like growth factor (IGF)-1 and IGF binding protein-3. J Natl Cancer Inst. 1999 7; 91 (7): 620-5.
Nicolucci A. Epidemiological and biochemical aspects of neoplasms in diabetes. Acta Diabetol 2010; 47: 87–95
Palmqvist R, Halmans G, Rinaldi S, et al. Plasma insulin-like growth factor, insulin-like growth factor binding protein, and colorectal cancer: a prospective study in Sweden. Gut 2002; 50: 642-6.
Prasad S, Gu X, Lipsitz SR, et al Effect of Depression on Diagnosis, Treatment, and Mortality of Men With Clinically Localized Prostate Cancer. JCO, 2014 JCO.2013.51.1048
Richardson LC and Pollack LA. Therapy insight: influence of type 2 diabetes on the development and outcomes of cancer. Nat Clin Pract Oncol 2005; 2:48-53
Ryan CJ, Hagg CM, Simko J, Nonaka DF, Chan JM, Weinberg V, et al. Expression of insulin-like growth factor-1 receptor in local and metastatic prostate cancer. Urol Oncol 2007;25:134 – 40.
Silbernagel G, Machann J, Unmuth S et al. Effects of 4-week very-high-fructose/glucose diets on insulin sensitivity, visceral fat and intrahepatic lipids: an exploratory trial. Br J Nutr. 2011;106:79-86
Song Y, Manson J, Buring J, et al. Associations of dietary flavonoids with risk of type 2 diabetes, and markers of insulin resistance and systemic inflammation in women: J. Am. Coll. Nutr. 2005;24:376–384.
Stocks T, Rapp K, Bjørge T, et al Blood Glucose and Risk of Incident and Fatal Cancer in the Metabolic Syndrome and Cancer Project (Me-Can): Plos 2010 DOI: 10.1371/journal.pmed.1000201
Sun Q, Wedick N, Tworoger S. et al Urinary excretion of select dietary polyphenol metabolites is associated with a lower risk of type 2 diabetes in proximate but not remote follow-up in a prospective investigation in 2 cohorts of US women. J. Nutr. 2015 doi: 10.3945/jn.114.208736.
Surmacz E. Obesity hormone leptin; a new target for breast cancer? Breast Cancer Res 2007; 9(1): 301.
Thompson L, Yoon I, Jenkins D et al Relationship between polyphenol intake and blood glucose response of normal and diabetic individuals. Am J Clin Nutr 1984 vol. 39 (5) 745-751.
Teras LR, Goodman M, Patel AV, Diver WR, Flanders WD, Feigelson HS. Weight loss and postmenopausal breast cancer in a prospective cohort of overweight and obese US women. Cancer Causes Control. 2011;22(4):573–9
Tunco I, Bacchotti T, Barden C. Polyphenol content of Fava bean enriched pasta reduced GI post ingestion. Functional Foods in Health and Disease. 2016; 6)5) 291-305
Wedick N, Pan A, Cassidy A, et al. Dietary flavonoid intakes and risk of type 2 diabetes in US men and women. Am. J. Clin. Nutr. 2012;95:925–933.
Welsh J, Sharma A, Abramson J et al Caloric sweetener consumption and dyslipidemia among US adults.2010 JAMA 21; 303(15),1490-7.
Xiao J and Hoegger P. Dietary polyphenols and type 2 diabetes: current insights and future perspectives. Curr Med Chem. 2015(1):23-8.
Yang J Chan D, Felix E et al A Sucrose-Enriched Diet Promotes Tumorigenesis in Mammary Gland in Part through the 12-Lipoxygenase (inflammatory) pathway. 2015 Cancer Res; 76(1); 24–29.
Yu H, Rohan T. Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst 2000; 92: 1472–89.
Wedick N, Pan A, Cassidy A, et al. Dietary flavonoid intakes and risk of type 2 diabetes in US men and women. Am. J. Clin. Nutr. 2012;95:925–933.
World Cancer Research Fund International. ‘Curbing global sugar consumption: Effective food policy actions to help promote healthy diets and tackle obesity’, 2015
WHO / Food and Agricultural Organization joint report. Carbohydrates in human nutrition. FAO Food Nutr Pap 1998; 66:1-140.
Zhang ZJ, Zheng Z, Kan H, et al. Reduced Risk of Colorectal Cancer With Metformin Therapy in Patients With T2DM. A meta-analysis. Diabetes Care 2011;34:2323-8.
[/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]
